Obstructive Sleep Apnea
The most common type of sleep apnea is caused by obstruction of the upper airway. It is characterized by repetitive pauses in breathing during sleep, despite the effort to breathe, and is usually associated with a reduction in blood oxygen saturation. These pauses in breathing called apneas, (literally, “without breath”), typically last 20 to 40 seconds.
Surprisingly, despite dozens or even hundreds of awakenings per night, most adults with obstructive sleep apnea (OSA) have no recollection of these events. In fact, often the only evidence of this serious condition might be daytime fatigue and reports of loud snoring from bed partners. However, most people with OSA usually have one or more of the following symptoms.
Do you have any of these symptoms?
- Excessive and inappropriate daytime sleepiness
- Loud snoring occurring virtually every night
- Apneas (pauses in breathing) witnessed by bed partner
- Episodes of waking at night feeling short of breath or gasping for air
- Insomnia
- Problems with memory and/or concentration
- Impotence
- Changes in mood, particularly depression
- Fatigue
Symptoms and Consequences
The following symptoms of obstructive sleep apnea (OSA) can significantly reduce a person’s quality of life. (In one study the reduction in quality of life with OSA was equivalent to that observed with diabetes or hypertension.1) Studies show OSA can raise your death risk by 46%. However, treatment can successfully reduce and even resolve these problems.
Sleepiness
Many people with OSA are excessively sleepy during the daytime. This can make it difficult to work, and can even lead to job loss. If you have OSA you might fall asleep while driving a car, watching television, reading, talking on the telephone, or even while eating a meal. People with OSA might not complain of sleepiness; they just think that they are “slowing down” and getting more tired as they get older.
Depression and Memory Problems
Depression is very common in people with untreated OSA. Frequently, people are treated for depression for years before anyone realizes that OSA is causing the depression. People with OSA can also have memory problems, difficulty concentrating, amnesia of events, and slower reaction times.
Safety
People with OSA are up to ten times more likely to have a motor vehicle accident as a result of sleepiness, sometimes with fatal results.5 Persons who knowingly drive while sleepy may be at risk for civil and criminal liability.6 OSA-related sleepiness can be especially devastating with commercial truck drivers (who have higher rates of OSA) as well as operators of public transportation vehicles. A 2008 train crash in Boston was attributed to the sleepiness of a driver who likely had undiagnosed OSA.7 In this sad example, the driver was killed, passengers were injured, and millions of dollars of damages were incurred.8
There is increasing evidence that untreated obstructive sleep apnea (OSA) can have a significant impact on your personal health. Successful treatment of OSA may reduce the risks of these related ailments.
Why does OSA increase the risk of having other health problems?
Studies suggest that having OSA raises the heart rate and increases blood pressure, placing stress on the heart. This may be because apneas frequently reduce blood oxygen levels, activating the branch of the nervous system responsible for increasing heart performance. In addition, levels of chemicals in the blood that cause inflammation and promote elevations in blood sugar rise. Such inflammation can damage the heart and blood vessels. 1, 2 Both hypertension and diabetes increase the risk for heart disease, and the likelihood of being diagnosed with one of these illnesses increases as a result of OSA.
Hypertension
High blood pressure is a common chronic medical condition. It afflicts over 40% of people between 50 and 60 years of age in the United States. OSA is a risk factor for the development of hypertension.3 Approximately 50% of those with sleep apnea have hypertension. In fact, elevated blood pressure might be the only clue that a person has OSA. Fortunately, treatment of OSA may result in better control or even resolution of hypertension.
Heart Disease
Coronary artery disease occurs in 67% of the adult population of the United States. It frequently results in heart attacks and premature death. Evidence indicates that OSA might be a risk factor for future heart attacks or angina pectoris (chest pain related to blockage of blood vessels supplying the heart), and middle-aged men might be at particular risk.
Stroke
Having a stroke can be a devastating event, with the potential for severe disability or death. OSA might be a risk factor for having a stroke and recovery after a stroke might be delayed in people with OSA. Conversely, people who have had a stroke are more at risk of developing OSA.
Diabetes Mellitus
Coinciding with the increase in obesity in the United States, more and more people are developing type 2 diabetes. Research indicates that blood sugar (glucose) levels are higher among people with OSA. However, it appears that treatment of OSA may improve blood sugar levels.
Premature Death
Because OSA is associated with a number of chronic medical conditions, not surprisingly, several studies have shown an association between OSA and increased likelihood of premature death.6 Middle-aged men appear to be at greatest risk, with the cause of death most commonly related to cardiovascular disease. Football star Reggie White, a Hall of Fame defensive end for three NFL teams, died of cardiac and pulmonary problems that were likely intensified by his sleep apnea. He was 43.
Obstructive Sleep Apena Treatment Options
Surgery
The intention of surgery is to create a more open airway so obstructions are less likely to occur. There are several different surgical procedures with different effectiveness rates. The most common surgery for sleep apnea is the uvulopalatopharyngoplasty, or UPPP procedure, which is intended to enlarge the airway by removing or shortening the uvula and removing the tonsils and adenoids, if present, as well as part of the soft palate or roof of the mouth. A tracheotomy–the surgical creation of a hole in the trachea or windpipe below the site of obstructions–is the most effective surgery for OSA. Unacceptable to most people, it is generally reserved for serious apnea that has failed other treatment. Other surgical procedures include maxillomandibular osteotomy or advancement (MMO or MMA) which try to enlarge the airway by moving the jaw forward.
CPAP
CPAP, or continuous positive airway pressure, is a treatment that uses constant air pressure to keep your airways open. The pressuer is constant, so a CPAP user cannot breathe through their mouth or the air will blow out. CPAP treatment is done using a CPAP machine. CPAP machines have three main parts:

- A mask or other device that fits over your nose or your nose and mouth
- Straps keep the mask in place while you’re wearing it
- A tube that connects the mask to the machine’s motor
- A motor that blows air into the tube
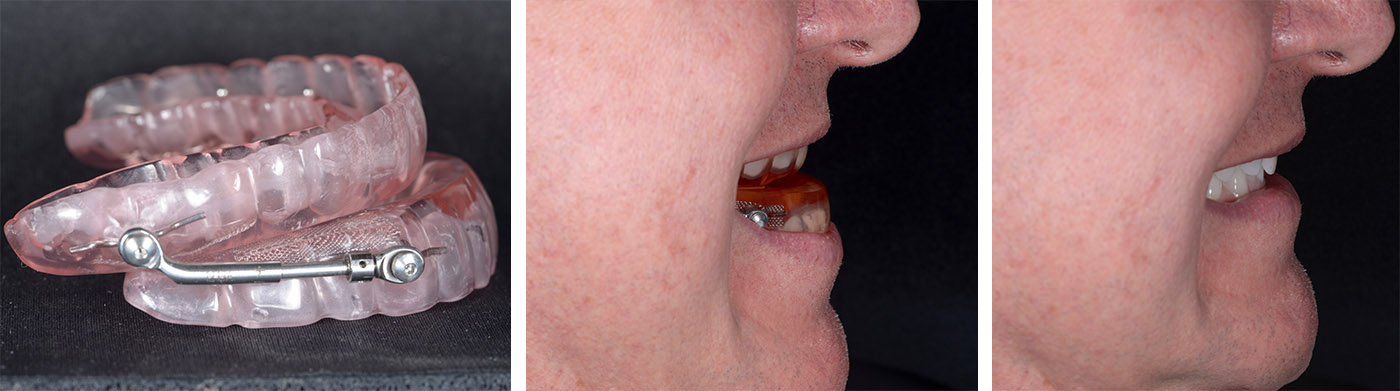
Oral Appliances
Intended to treat apnea by keeping the airway open in one of three ways: by pushing the lower jaw forward (a mandibular advancement device), by preventing the tongue from falling back over the airway (a tongue-retaining device), or by combining both mechanisms. Oral appliances are typically more effective for people with mild sleep apnea but can, for some, be effective for moderate and severe sleep apnea. Appliances are often adjustable so that the dentist can move the jaw further or reduce the advancement as necessary. The goal is to find the most comfortable and effective position for the patient.
References
- Baldwin CM, Griffith KA, Nieto FJ, O’Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the sleep heart health study. Sleep 2001;24:96-105.
- AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnea. Lung 2008;186:7-12.
- Harvard Medical School Division of Sleep Medicine. The price of fatigue. December, 2010. http://sleep.med.harvard.edu/what-we-do/public-policy-research
- Peker Y, Hedner J, Johansson A, Bende M. Reduced hospitalization with cardiovascular and pulmonary disease in obstructive sleep apnea patients on nasal CPAP treatment. Sleep 1997; 8:645-53.
- George CF. Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med 2007;176:954-6.
- Madigan E. New Jersey cracks down on drowsy driving. Stateline, November 18, 2003.Link
- Czeisler CA. Drowsy-driving tragedies preventable. Boston Globe, August 3, 2009. Link
- Chakrabarti M. NTSB faults T safety systems in deadly T crash. WBUR, July 15, 2009. Link
Above information, with permission from Harvard University.
A resource from the Division of Sleep Medicine at Harvard Medical School.
Produced in partnership with WGBH Educational Foundation.
Book your appointment today
Booking your appointment is easy, and our dedicated staff is here to help you every step of the way.

